Hey there!
I often get asked the question “when” in two very different ways from my patients, and I want to take a moment to chat about it. The first way comes from a place of acceptance. These are the folks who understand they have an injury and know that with the right information and a solid rehab plan, they’ll be back to their favourite activities in no time. It’s like they’re saying, “I get it, and I’m ready to do what it takes!”
Then there’s the second group, and I totally get where they’re coming from. These patients often ask “when” from a place of panic and despair. They might not have played competitive sports before, but they’re feeling the weight of not being able to join their beloved exercise classes. You can almost see the wheels turning as they negotiate with me about when they can return, creating a whirlwind of anxiety in the process. It’s not uncommon for the first part of our session to be about helping them calm down and find their center.
Now, you might think I lack empathy for these patients, but that couldn’t be further from the truth! Many of them attend these classes for deeply personal reasons, and mental health is often at the top of that list. I completely understand how the panic can set in when they feel like they’re missing out on something that brings them joy and stability.
But here’s the good news: I’m here to help all my patients become pain-free and get back to their chosen activities as soon as possible! Yes, like everyone else, I do have bills to pay, and the longer it takes to heal, the more I might earn. But honestly, that’s not my goal! The quicker you heal and feel great, the more likely you are to share your positive experience with others, and that’s what truly matters to me.
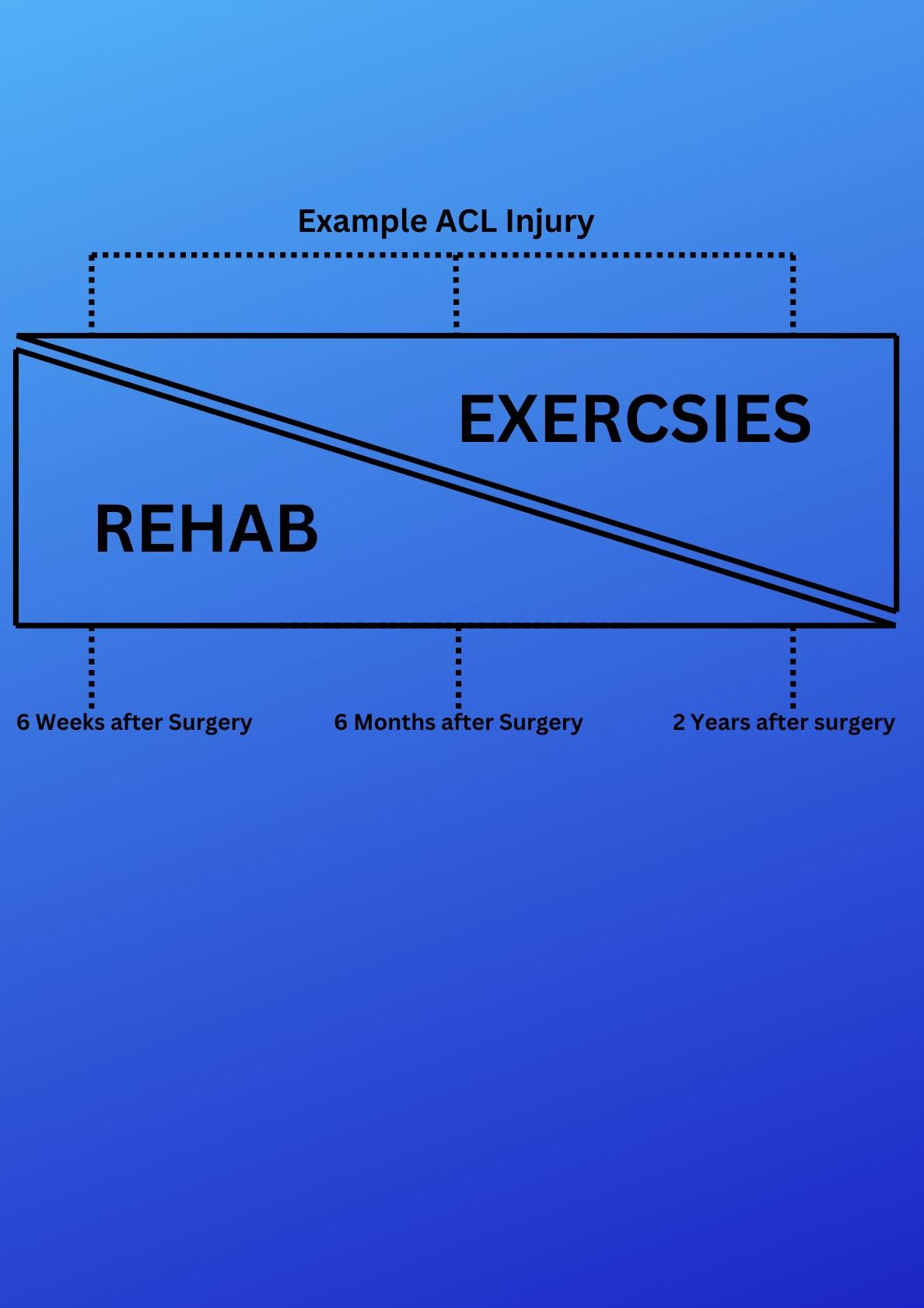
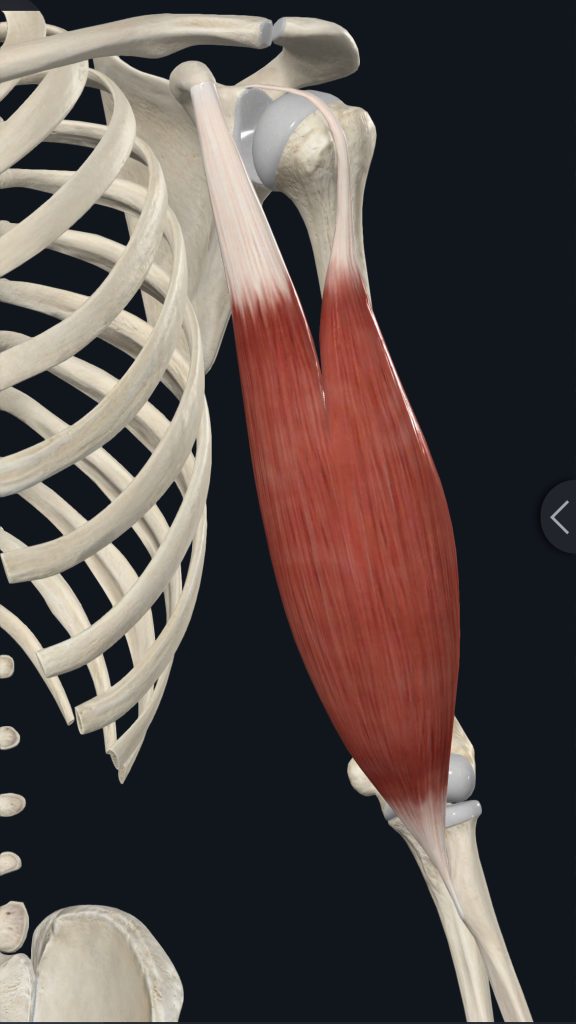
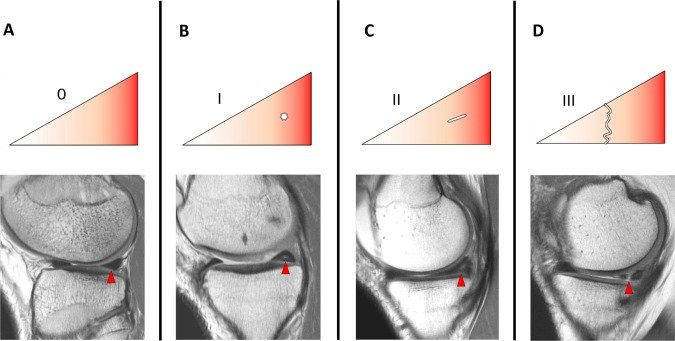
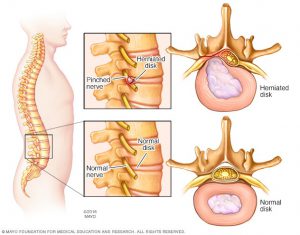
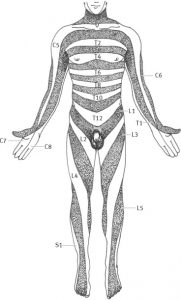
The diagram above illustrates a typical recovery timeline for an ACL injury over a two-year period. It’s important to note that the severity of an injury directly impacts healing time. For instance, while an ACL injury might take up to two years to fully recover, a less severe injury, like a muscle strain, could heal in as little as two months. In fact, many people can return to their workout classes just 2 to 4 weeks after a muscle strain!
The key takeaway here is: don’t despair! We’re all human, and the body has its own natural healing pace depending on the type of injury. While it can be frustrating, the best approach is to accept where you are in your recovery journey, focus on the right rehabilitation exercises, and work towards getting back to your favorite activities as soon as possible. Thanks for taking the time to read this!